Suturing wounds is a common surgical procedure, but some patients may experience slow or even non-healing wounds. This not only prolongs recovery time but also increases the risk of infection. Below, we share information on chronic wound healing and proper postoperative care.

What factors can affect wound healing?
- Infection is the most common cause. Bacteria multiplying in the wound produce toxins that destroy new granulation tissue, leading to redness, swelling, and purulent discharge at the suture site. Excessive wound tension can also impair healing, especially in wounds involving joints or larger skin defects, where the traction generated by daily activities can separate the wound edges. Insufficient blood supply is also important. Areas with thick subcutaneous fat or those that have been treated with radiation have poor blood supply, significantly slowing healing. Retained foreign matter, such as suture reactions, gauze fibers, or metal fragments, can also lead to persistent inflammation in the wound.
- Systemic factors should also not be ignored. Malnutrition, especially protein deficiency, prevents the body from providing sufficient raw materials to repair tissues. Insufficient vitamin C and zinc can also delay collagen synthesis. When diabetic patients have poor blood sugar control, high blood sugar levels can impair vascular function, affect white blood cell activity, and significantly reduce healing capacity. Elderly people experience poor blood circulation and weakened cell regeneration, so wound healing naturally slows. Nicotine in smokers causes blood vessels to constrict, reducing oxygen supply to tissues, while carbon monoxide reduces the oxygen-carrying capacity of red blood cells. Certain medications, such as hormones and chemotherapy drugs, can also inhibit cell division and inflammatory responses.
How to determine poor wound healing?
A normally healing wound begins to show pink granulation tissue 5-7 days after surgery, with well-aligned edges and no noticeable exudate. A poorly healing wound, on the other hand, may experience dehiscence after suture removal or persistent exudation of bloody or purulent secretions. The wound edge may appear whitish or dark purple and feel cold to the touch, indicating poor local blood supply. Sometimes a layer of yellow necrotic tissue forms on the wound surface, hindering the growth of new epithelium. Patients may experience persistent pain or distension, and the surrounding skin may become more red and swollen.
How to promote wound healing?
For localized infections, prompt wound debridement is necessary to remove necrotic tissue and pus. Based on bacterial culture results, sensitive antibiotics should be administered, and if necessary, some sutures should be removed to facilitate drainage. If wound tension is excessive, consider using tension-relieving sutures or tape to restrict local movement. For areas with poor blood supply, ointments that promote blood circulation, such as growth factor gel, can be used. Any remaining foreign body must be thoroughly debrided and removed.
Regarding systemic factors, those with malnutrition should increase their protein intake, eat more fish, meat, eggs, dairy products, and soy products, and take appropriate vitamin C and zinc supplements. Diabetics should strictly control their blood sugar, ideally keeping their glycosylated hemoglobin below 7%. Smokers must quit smoking at least until the wound is fully healed. Elderly individuals should take special care to keep the wound clean and dry, avoiding pressure.
When should you seek professional help?
If the wound is noticeably red, swollen, hot, painful, has purulent discharge or a foul odor, or has a temperature exceeding 38°C, seek medical attention immediately. If the wound continues to bleed or is significantly open, seek medical attention . Early medical intervention is recommended for patients with diabetes, weakened immune systems, or if the wound is located in a vital area such as the face.
What are the modern wound treatment methods?
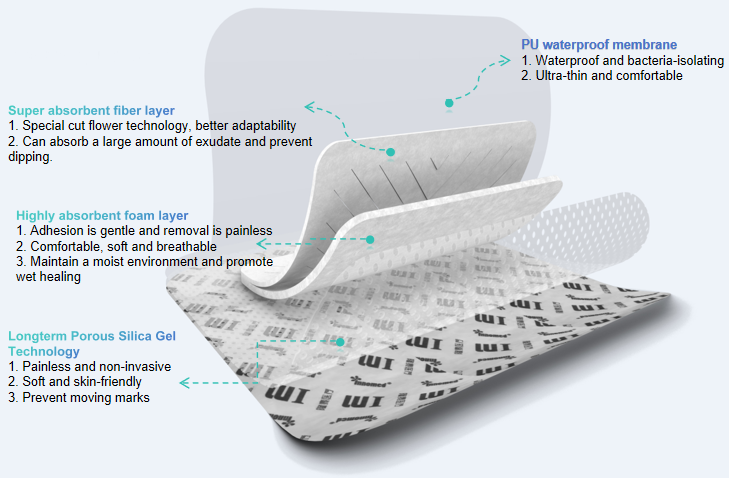
Negative pressure wound therapy uses specialized equipment to generate negative pressure on the wound surface, promoting the growth of granulation tissue. Hyperbaric oxygen therapy increases tissue oxygen content and enhances the bactericidal ability of white blood cells. Various new dressings, such as hydrocolloid dressings, alginate dressings, and silver ion dressings, can provide a suitable healing environment for wounds. Growth factor preparations directly stimulate cell proliferation and accelerate the healing process. For large skin defects, flap transplantation or skin grafting may be necessary.
For more information on Innomed®Super Absorbent Non-adhesive, refer to the Previous Articles. If you have customized needs, you are welcome to contact us; You Wholeheartedly. At longterm medical, we transform this data by Innovating and Developing Products that Make Life easier for those who need loving care.
Editor: kiki Jia

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








