Skin flap transplantation is a commonly used technique in plastic surgery and trauma repair, but postoperative tissue devitalization can occur in the transplanted area. This condition manifests as darkening of the flap, decreased temperature, loss of capillary reactivity, and, in severe cases, tissue necrosis. Proper management of devitalization in the surgical area is crucial to preserving the transplant outcome, and staged treatment measures are required based on the degree of devitalization.

How to determine whether the flap has devitalized?
Skin flap devitalization usually has clear clinical manifestations. Early on, the flap's color changes from its normal rosy red to pale or cyanotic, and when touched, its temperature is significantly lower than that of the surrounding normal tissue. Gentle pressure with a cotton swab can cause a slow or complete loss of capillary refill. As the disease progresses, the devitalized area gradually darkens and hardens, forming a clear boundary with the surrounding healthy tissue. The patient may experience local numbness or increased pain. Ultrasound Doppler examinations can reveal a weakened or absent blood flow signal in the flap. Clinically, devitalization is divided into complete and partial devitalization, with the former involving the entire flap and the latter limited to a local area. Timely and accurate judgment is crucial for the selection of subsequent treatment options.
How should we deal with the early stage of devitalization of the surgical area?
The focus of the initial treatment of inactivation is to control infection and remove necrotic tissue. The use of silver ion dressings is an effective means of controlling infection. Silver ions can penetrate the bacterial cell wall, interfere with its metabolic process, and have a significant inhibitory effect on common pathogens such as Staphylococcus aureus and Pseudomonas aeruginosa. At the same time, it is necessary to use external preparations with detoxification and myogenic effects. Such drugs usually contain a variety of traditional Chinese medicine ingredients, which can promote the dissolution and shedding of necrotic tissue and reduce local inflammatory reactions. During debridement, special attention should be paid to protecting tissues that have not been completely inactivated. A conservative debridement strategy should be adopted to gradually remove the clear necrotic parts in stages. At this stage, the wound should be kept moderately moist to avoid secondary damage caused by drying. Hydrogel dressings can be used to maintain the wound microenvironment.
How to promote the growth of granulation tissue in the devitalized area?
When the infection is under control and the necrotic tissue is cleared, the focus of treatment shifts to promoting the formation of granulation tissue. Growth factor gel is the core treatment method at this stage, and commonly used ones include recombinant human epidermal growth factor, basic fibroblast growth factor, etc. These bioactive substances can stimulate fibroblast proliferation and capillary regeneration, accelerating the filling of granulation tissue on the wound surface. When used, it needs to be applied evenly to the base of the wound and maintained for an appropriate contact time. The use of negative pressure wound treatment technology can further improve local blood flow, reduce exudation, and promote the healthy growth of granulation tissue. Nutritional support is equally important. Patients need to increase their protein intake, at least 1.5 grams per kilogram of body weight per day, and supplement with sufficient vitamin C and zinc. At this stage, the quality of granulation tissue should be closely observed. Healthy granulation tissue should be bright red, uniform in particles, and easy to bleed when touched.
In what situations should secondary surgical intervention be considered?
Not all flap devitalization can be resolved through conservative treatment. When the range of devitalization exceeds 30% of the flap area or involves critical functional areas, secondary surgery needs to be considered. Deep tissues such as muscles and tendons are exposed and cannot be covered by granulation tissue, surgical intervention is also required. Surgical methods include local flap readjustment, free skin grafting, and even flap redesign. A comprehensive assessment of the patient's general condition and local blood supply conditions is required before surgery, and angiography should be performed if necessary. The timing of the secondary surgery is critical, and it is usually performed after the infection is completely controlled and the boundaries of necrosis are clear. Postoperative monitoring should be strengthened to prevent the recurrence of circulatory disorders.
How to prevent devitalization after flap transplantation?
Preventive measures should be implemented throughout the perioperative period. The patient's vascular condition should be fully assessed before surgery, and smokers should quit smoking for at least two weeks. Intraoperative manipulation should be delicate, avoid excessive traction and compression of the flap, and pay attention to protecting the vascular pedicle. Maintain a proper body position after surgery to avoid compression or twisting of the vascular pedicle. Maintain the ambient temperature at 24-26 degrees Celsius to prevent vasospasm. Routinely use anticoagulants and vasodilators, such as low molecular weight heparin and prostaglandin E1. Closely monitor the color, temperature, tension, and capillary response of the flap, and establish an hourly recording system. Pain management should be in place to avoid vasoconstriction due to pain. The period within 72 hours after surgery is a high-incidence period for vascular crisis and requires special attention.
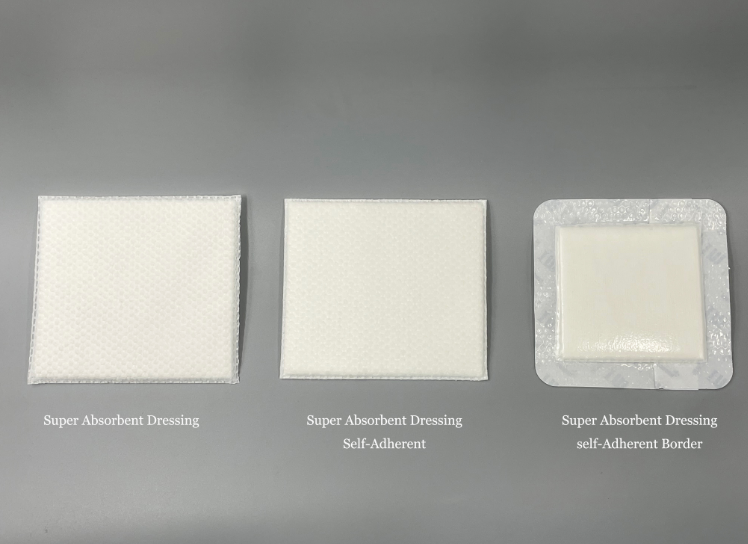
Devitalization of the surgical site after flap transplantation is a serious complication, but early identification and standardized management can often salvage the graft. Treatment requires a phased approach, initially focusing on infection control and debridement of necrotic tissue, followed by the promotion of granulation. When conservative treatment fails, surgical intervention should be considered promptly. Preventive measures should begin preoperatively and continue throughout the treatment process. Healthcare professionals must master flap monitoring techniques, while patients and families must understand basic care. Multidisciplinary collaboration and personalized care are key to successfully managing flap devitalization. Advances in biomaterials and regenerative medicine may provide more effective solutions to this challenge. For more information on Innomed® Silver Ion Dressing Textile Fiber, refer to the previous article. If you have customized needs, please contact us; we will wholeheartedly. At longterm medical, we transform this data by innovating and developing products that make life easier for those who need loving care.
Editor: kiki Jia

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








