When an open wound is present, maintaining a balance between personal hygiene and wound protection becomes a crucial aspect of daily care. While showering is a basic cleansing requirement, special precautions are required when a wound is present to ensure effective cleaning while preventing infection and impeded healing.
What types of wounds can be showered?
Superficial abrasions and cuts can usually be covered with proper protection. These wounds are shallow and pose a relatively low risk of contamination. Sutured surgical wounds require evaluation before suture removal. Showering is generally permitted 24-48 hours after surgery, after initial wound closure. Chronic wounds with well-developed granulation tissue may be allowed to shower after a physician's evaluation. After blood flow to the grafted area or flap is established and stabilized, showering may be permitted as directed by the physician.
When should you avoid showering?
Avoid showering if the wound shows obvious signs of infection, including increased redness, swelling, purulent discharge, and fever. Wounds that expose deep tissue, such as those with visible tendons, bones, or internal organs, must be kept dry. Wounds that have just had their dressings changed or have been treated with special ointments should be kept dry for a fixed period of time as directed by the doctor. Patients with severely compromised immune systems should avoid showering with any open wounds. Showering is strictly prohibited during the early healing phase of skin flaps or grafts without an established blood supply.
What preparations should you make before taking a shower?
Choose a professional waterproof dressing, ensuring it completely covers the wound and extends 2-3 cm beyond the edges. Check the waterproof dressing packaging to confirm the expiration date and integrity. Prepare sterile gauze and tape as backup protective measures. Adjust the bathroom temperature to avoid excessive cold that causes muscle tension or excessive heat that increases sweating. Keep clean towels and clothing readily accessible. Limit showers to 5-10 minutes to minimize the time the wound is exposed to moisture.
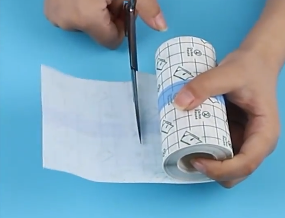
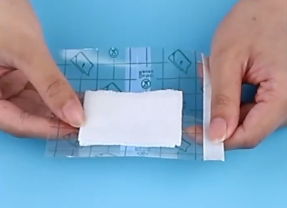
How to use waterproof protection measures correctly?
Clean the skin around the wound and ensure it is dry and free of grease to ensure a secure fit for the waterproof dressing. Start applying the waterproof dressing from one side and gradually work your way toward the other side, avoiding wrinkles. Press the edges of the dressing with your palms, especially around active areas, to ensure a complete seal. Create a closed, waterproof barrier around the wound. When showering, avoid direct water flow to the protected area. Use an elastic bandage for additional securement around joints to prevent the edges of the dressing from lifting due to movement.
What should you pay attention to when taking a shower?
Use lukewarm water, not hot water; excessively hot water may break down the waterproof dressing and irritate the wound. Avoid using shower gel or soap directly on the wound area, as the chemicals may seep through the edges of the dressing. Maintain a normal shower posture and avoid excessive stretching or bending, which can cause the dressing to shift. Move gently and avoid sudden turns or large movements. Stop showering immediately if you feel water seeping around the edges of the dressing.
What should I do after showering?
First, dry the rest of your body with a dry towel, then treat the wound area last. Gently peel back the waterproof dressing from the edges toward the center, taking care not to pull on the wound. Inspect the inner layer of the dressing for water seepage, and record and observe the wound. Use sterile gauze to dry the skin around the wound and keep it dry. Replace the wound dressing as directed by your doctor, carefully observing the wound for any abnormal changes. Record the wound's reaction after showering to provide a reference for subsequent care.
When should you stop showering?
If the waterproof dressing has a poor seal and leaks repeatedly, discontinue use. If the wound develops new pain, redness, swelling, or increased exudate, or if the patient experiences discomfort such as dizziness or fatigue, they should not shower alone. If the water temperature cannot be stably controlled, it creates a risk of burns. If the wound is mobile and cannot be effectively waterproofed.
What are the key points to observe for wounds after showering?
Inspect the wound edges for whitening or maceration, which indicates excessive moisture. Observe changes in the amount, color, and odor of exudate absorbed by the dressing. Note any new rash or itching on the surrounding skin, which may be an allergic reaction to the waterproofing material. Feel around the wound for localized warmth. Compare the size and depth of the wound before and after showering.
For more information on Innomed®Transparent Dressing Green-Squares, refer to the Previous Articles. If you have customized needs, you are welcome to contact us; You Wholeheartedly. At longterm medical, we transform this data by Innovating and Developing Products that Make Life easier for those who need loving care.
Editor: kiki Jia

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








