Correctly assessing wound condition and taking effective preventive measures are crucial aspects of wound management. Through systematic observation and scientific methods, wound status can be accurately assessed, the risk of complications can be reduced, and the healing process can be accelerated.
How to comprehensively assess the wound condition?
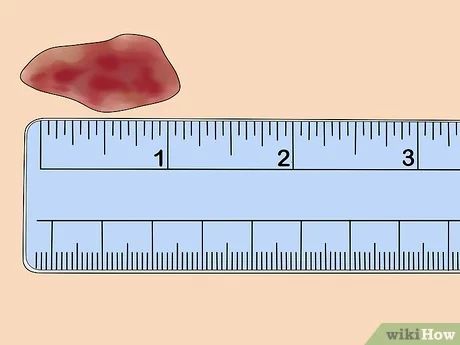
Observing the appearance of the wound is a basic assessment step. Pay attention to the size, depth, and edge morphology of the wound, and measure and record the specific dimensions. Observe the color of the underlying tissue. Healthy granulation tissue is bright red, yellow indicates the presence of slough, and black indicates necrotic tissue. Check the exudate, including the amount, color, viscosity, and odor. Clear, light yellow exudate is normal, while turbid, purulent exudate may indicate infection. Assess the condition of the surrounding skin, paying attention to redness, swelling, heat, nodules, or maceration. Understand the patient's pain level and record it using a numerical scoring method. Also, ask about the cause and duration of the wound, as this information is important for determining the prognosis.
How to recognize signs of infection?
Local infection manifests as increased redness and swelling, increased pain, and skin temperature. The exudate changes in nature, becoming purulent and increasing in volume, possibly with an unpleasant odor. Redness, swelling, and infiltration may develop around the wound margins, potentially leading to the formation of new abscesses. Systemic symptoms such as fever, chills, and fatigue suggest the possibility of widespread infection. Laboratory tests reveal elevated white blood cell counts and C-reactive protein levels. The culture of wound secretions can identify the causative bacteria.
What factors affect wound healing?
Systemic factors include age, nutritional status, and underlying medical conditions. Healing is slower in the elderly, and malnutrition, particularly protein deficiency, can delay repair. Conditions such as diabetes, anemia, and immunosuppression can also affect healing. Long-term use of glucocorticoids or immunosuppressants can also slow healing. Local factors, such as the blood supply to the wound site, are crucial; areas with a rich blood supply heal faster. Foreign matter, necrotic tissue, and hematoma formation within the wound can impede healing. Excessive local pressure or persistent friction can also impair the healing process.
How to properly clean and protect wounds?
Before cleaning the wound, wash your hands and prepare sterile instruments and dressings. Irrigate the wound with normal saline to remove surface contaminants and bacteria. Disinfect from the center outward to avoid introducing surrounding bacteria into the wound. Choose an appropriate dressing based on the wound's condition. Exudate-prone wounds should use a highly absorbent dressing. Dry wounds should maintain a moist environment. Change the dressing regularly and monitor the wound for changes. The frequency of change should be determined by the amount of exudate; avoid frequent changes that may damage new tissue.
What preventive measures can reduce the occurrence of wounds?
Keep your skin clean and dry, especially in wrinkles and pressure areas. Use a mild cleanser and avoid over-degreasing. Apply moisturizer promptly after showering to maintain the skin's barrier function. Avoid prolonged pressure, change body positions regularly, and use pressure-relieving pads to protect bony prominences. Wear appropriate footwear and socks to avoid friction and pressure. Pay attention to environmental safety to prevent accidental injuries. Enhance nutritional intake to ensure adequate protein, vitamins, and trace elements.
How to treat special types of wounds?
For pressure injuries, the key is to relieve pressure, turn the patient regularly, and use a specialized pressure-relieving mattress. Diabetic foot ulcers require strict blood sugar control, appropriate footwear, and daily foot checks. Venous ulcers require pressure therapy, elevating the affected limb to promote venous return. Arterial ulcers require improved blood supply, avoiding weight bearing, and protecting the affected limb. Burn wounds require careful attention to infection prevention and maintaining fluid and electrolyte balance.
For more information on Innomed®Hydrocolloid Dressing Ultra-thin, refer to the Previous Articles. If you have customized needs, you are welcome to contact us; You Wholeheartedly. At longterm medical, we transform this data by Innovating and Developing Products that Make Life easier for those who need loving care.
Editor: kiki Jia

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








