Why is a stoma assessment necessary?
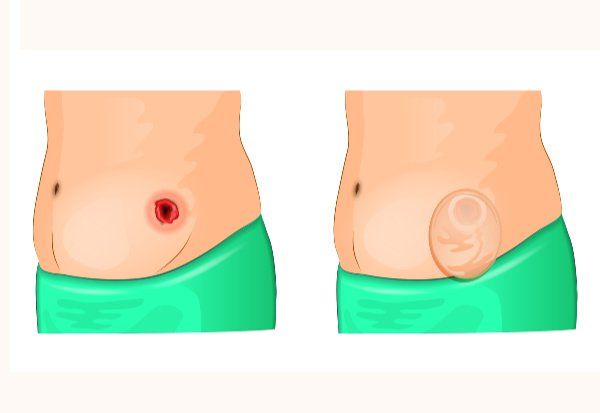
Stoma assessment is a crucial part of stoma care, far more than a simple routine check; it's a core component of postoperative recovery and long-term life management. Its primary purpose is to detect complications early. By systematically observing the stoma's color, shape, size, height, and the condition of the surrounding skin, caregivers or the patient can identify problems such as ischemia, retraction, prolapse, parahernia, or irritant dermatitis early, allowing for timely intervention and preventing minor issues from escalating into more serious conditions requiring reoperation. Secondly, assessment reveals the recovery of stoma function. By observing the characteristics, color, and amount of gas and excrement from the stoma, it's possible to determine if bowel function has recovered smoothly. This provides a direct basis for subsequent dietary adjustments, activity guidance, and the development of an overall rehabilitation plan. Ultimately, all assessment information is compiled into a clear record to guide every subsequent nursing decision and treatment adjustment.
What exactly does an ostomy assessment include?
A complete stoma assessment requires observing the color of the stoma mucosa. A healthy color should be a moist, bright red or pink, similar to the oral mucosa. A dark red, purple, or pale color suggests potential blood supply problems. Observe the shape of the stoma—whether it is round, oval, or irregular—as this directly affects the shape of the stoma baseplate. Accurately measure the size using a specialized measuring ruler, noting the major and minor axes of the stoma base, usually in millimeters. This is because the stoma size may change monthly during the early postoperative period due to swelling reduction. Assess the stoma height; ideally, it should protrude 1 to 2 centimeters above the skin surface. Too high, and it's prone to friction; too low, and leakage is likely. Carefully examine the skin around the stoma for signs of redness, breakage, rash, or fungal infection. Finally, perform a functional assessment, recording the nature, frequency, and amount of excretions, as well as any discomfort such as abdominal distension or pain.
How to select nursing supplies based on assessment results?
The direct application of stoma assessment is guiding the selection of nursing supplies, which directly affects the patient's quality of life. Based on the measured stoma size and shape, the opening of the stoma baseplate is selected or cut. In principle, the opening should be 1 to 2 millimeters larger than the stoma base to ensure a snug fit without compressing the mucosa. A convex or flat baseplate is selected based on the stoma height. For flush or recessed stomas, a baseplate with a convex ring may be needed to ensure a tight seal and prevent leakage. The type of ostomy bag is selected based on the characteristics of the excrement. For ileostomies with thin excrement, an open bag should be selected and used with a leak-proof ointment; for colostomies with formed excrement, a closed bag can be chosen. Additional products are selected based on the condition of the surrounding skin. If the skin is red and broken, stoma powder and skin protectant can be used; if there are depressions or wrinkles, leak-proof strips or ointment should be used for filling. A truly suitable set of nursing supplies should ensure a secure fit, a good seal, and no skin irritation.
How to develop an individualized stoma care plan?
Every individual's physical condition, medical condition, and lifestyle are different; therefore, stoma care plans must be individualized. The development of a plan requires comprehensive information, including whether the patient's underlying disease is cancer or inflammatory bowel disease, which determines the long-term expected bowel function. The patient's age, physical strength, vision, and hand dexterity directly affect their self-care ability. Abdominal shape, the presence of scars or folds, determines the difficulty of attaching stoma supplies. Simultaneously, the patient's psychological state, family support, and financial situation are also crucial factors. Based on a comprehensive assessment, the care plan will detail the daily care routine, change frequency, dietary and hydration recommendations, suitable exercise methods, and procedures for handling common problems. This plan is not static; it will be dynamically adjusted as time progresses post-surgery, the patient's physical condition changes, and assessment results are updated.
How can we evaluate the effectiveness of nursing care through assessment?
Regular, standardized stoma assessments serve as a benchmark for evaluating the effectiveness of treatment and nursing interventions. By comparing records from previous assessments, trends can be objectively observed. For example, has the persistent rash around the stoma been relieved after using a new skin protectant? Has recurrent leakage ceased after changing to a convex baseplate? Has the patient's reported itching or pain been alleviated after targeted measures were taken? Regarding functional recovery, observations can be made of whether bowel movements and gas become more regular and whether abdominal distension is reduced. More importantly, improvements in the patient's quality of life are crucial, such as increased confidence in ostomy bag changes, greater freedom of daily activities, and reduced anxiety. If the assessment reveals that expected goals have not been achieved, such as unresolved complications or the emergence of new problems, a timely review is necessary. Discussions with the doctor and stoma therapist are needed to adjust the nursing plan or treatment strategy until the best care outcome is achieved.
What key points should patients pay attention to during self-assessment?
For patients requiring long-term self-management, mastering correct self-assessment methods is crucial. A quick observation should be performed daily when changing the ostomy bag, noting any sudden darkening of the stoma color or new skin breakdown or severe redness around the stoma. Check the stability of the baseplate attachment and for frequent leakage, which may indicate a change in stoma size or that the baseplate type is no longer suitable. Pay attention to abnormal changes in excretions, such as sudden watery stools, diarrhea, or no gas or stool for more than 48 hours. Heed warning signs from the body, such as unusual abdominal cramps, severe pain in the stoma area, unexplained fever, or large amounts of bright red blood flowing from the stoma . For more information on Innomed® Ostomy Pouch , refer to the Previous Articles. If you have customized needs, you are welcome to contact us; You Wholeheartedly. At long-term medical, we transform this data by Innovating and Developing Products that Make Life easier for those who need loving care.
Editor: kiki Jia

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








