What is a pressure injury?
Pressure injuries, formerly known as bedsores or pressure ulcers, refer to localized damage to the skin and subcutaneous soft tissues caused by prolonged pressure, or pressure combined with shear forces. These injuries typically occur at bony prominences, such as the sacrum, heels, and hips. The root cause is that continuous pressure obstructs local blood flow, leading to tissue ischemia and hypoxia, ultimately resulting in cell death and tissue damage. Pressure injuries are not simply skin breakdowns; they begin in deeper tissues. Sometimes the epidermis appears intact, but the subcutaneous tissue has already necrotized, which is the dangerous aspect. Based on the depth of tissue damage and clinical manifestations, an internationally recognized staging system is used to describe the severity of these injuries.
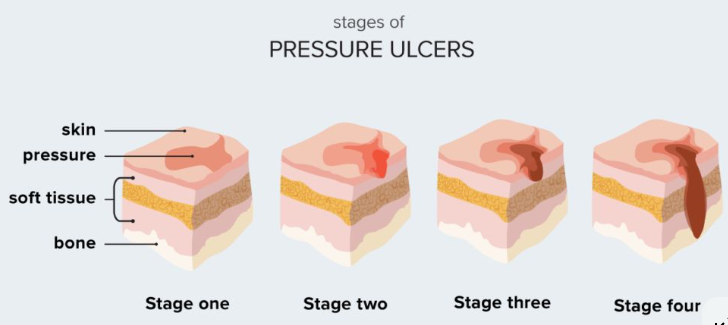
What are the specific stages of pressure injury?
Pressure injuries are currently classified into six stages. Stage 1 pressure injury is the earliest sign, presenting as an intact patch of skin that does not turn white upon pressure. In individuals with darker skin tones, it may appear as a color change different from the surrounding skin, such as purple or brownish-red. This area may be painful, hard or soft, and hotter or cooler than the surrounding skin. Stage 2 injury involves partial loss of skin, presenting as a superficial open ulcer with a pink or red wound surface and no slough. It may also present as an intact or ruptured serous vesicle. Stage 3 injury involves full-thickness skin loss, with subcutaneous fat visible, but bone, tendons, or muscles are not yet exposed. Slough may be present, and the depth of the wound varies depending on the anatomical location. Stage 4 injury is the most severe, with full-thickness skin and tissue loss, exposing bone, tendons, or muscles. The wound base is often covered with slough or eschar. In addition, there are two special types: unstageable injuries and deep tissue injuries.
Why is it that sometimes the epidermis is intact but it is diagnosed as deep tissue damage?
This is a crucial yet easily overlooked issue in pressure injuries. Deep tissue injury is a special type, characterized by intact skin that turns purple or brownish-red, or develops congested blisters. This occurs because the injury begins in the deep muscle layer and progresses outwards. When deep muscles and soft tissues undergo ischemic necrosis due to sustained pressure, the surface skin may temporarily remain intact due to the different blood supply. Upon touch, this area may feel harder or softer than the surrounding tissue, and there may be a temperature difference; the patient often experiences pain. This condition is extremely dangerous because the internal tissue has already necrotized. Even if the surface skin remains intact, the injury is quite severe and may rapidly develop into an open ulcer within a short period. Therefore, nursing care must not only focus on the skin surface but also pay attention to the local color, temperature, texture, and the patient's subjective symptoms.
What exactly does "irreversible injury" mean?
Unstageable injuries refer to the loss of full-thickness skin and tissue, but the wound base is completely covered by slough or eschar, making it impossible to determine the actual depth. Eschar is typically yellow, brownish, or black necrotic tissue, and its texture may be soft or hard like leather. Slough is yellow or yellowish-brown soft necrotic tissue. In this situation, the true wound depth is obscured by this necrotic material; it could be stage 3, stage 4, or even reach the bone. Therefore, accurate staging is impossible until sufficient slough or eschar is removed through debridement to expose the wound base. Clinically, the primary task in managing unstageable injuries is often planned debridement, rather than forced staging. Only after debridement can accurate staging be performed based on the exposed tissue type.
What are the different processing principles for different stages?
The core purpose of wound staging is to guide treatment, and the focus of management differs significantly between stages. For stage 1 injuries, the key is to relieve pressure, increase turning and repositioning, use pressure-reducing pads, protect the skin from moisture and friction, closely monitor changes, and prevent progression. The focus of stage 2 wound management is to protect the wound surface and prevent infection. This is typically achieved using moderately moist dressings such as hydrocolloid or film dressings to promote epithelial growth, while continuing to strengthen pressure-reducing measures. Stage 3 and 4 injuries are more complex to manage due to their depth, often requiring intervention from a specialized wound care nurse or physician. Core measures include thorough debridement, removal of necrotic tissue, infection control, exudate management, and promotion of granulation tissue growth. Depending on the wound condition, different types of dressings may be needed, such as alginate, foam, or silver-containing dressings. For extremely deep wounds, negative pressure wound therapy may be an option. Regardless of the stage, systemic supportive care is indispensable, including improving nutritional status, correcting anemia, and controlling pain.

What can family members do in prevention and care?
Family involvement is crucial for the prevention and early detection of pressure injuries. First, assist patients in changing positions regularly; bedridden patients should be turned at least every 2 hours, and wheelchair users should decompress every 15-30 minutes. Second, carefully examine the skin around bony prominences daily, especially the sacrum, heels, hips, and elbows, observing for any changes in color, blisters, ulceration, or changes in local temperature or firmness. Keep the skin clean and dry, avoiding immersion in urine or feces, and use mild cleansers and moisturizers. Ensure bed sheets are smooth and wrinkle-free, and clothing is soft and breathable. Provide patients with a balanced diet, especially ensuring sufficient protein and vitamin intake, which is fundamental for maintaining healthy skin. If any suspicious skin changes are observed, inform healthcare professionals promptly; do not massage reddened areas or apply folk remedies.
Will the staging be reversed after the wound heals?
This is a common misconception. Staging of pressure injuries describes the deepest level of tissue damage and is not reversible. That is, after a stage 4 injury heals, we don't say it has reverted to stage 1. As the wound heals, granulation tissue fills the wound, epithelium creeps over it, and the wound gradually shrinks, becomes shallower, and eventually closes. We track healing progress by describing specific indicators such as wound size, depth, exudate volume, and the proportion of granulation tissue. For example, we can say that a stage 4 wound has 75% red granulation tissue filling the base, its depth has decreased by 50%, and its area has shrunk by 30%. Clinical records will describe these dynamic changes in detail without altering the initially established stage. Understanding this helps in objectively assessing the effectiveness of care interventions and avoids misunderstandings caused by the perceived invariance of stage. For more information on Innomed® Silicone Foam Dressing , refer to the Previous Articles. If you have customized needs, you are welcome to contact us; You Wholeheartedly. At long-term medical, we transform this data by Innovating and Developing Products that Make Life easier for those who need loving care.
Editor: kiki Jia

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








