What are the common causes of poor wound healing after suturing?
Poor wound healing, medically termed delayed healing or poor healing, is often not caused by a single factor but rather by a combination of interrelated factors. Successful wound healing depends on a sophisticated physiological repair process, and any local or systemic factor that disrupts this process can cause problems. From the condition of the wound itself to the patient's overall health and the details of daily care, every aspect can be crucial in influencing healing. Understanding these causes is the first step in addressing the problem and promoting eventual wound healing.
What local wound factors can hinder healing?
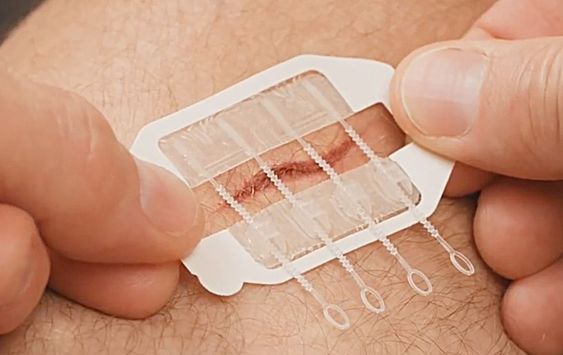
The condition of the wound itself is fundamental to healing. The most common and direct cause is infection. If the wound is not thoroughly cleaned during suturing, or if improper postoperative care allows bacteria to invade, infection will continuously produce an inflammatory response, consuming a large amount of repair resources and releasing toxins that damage newly formed tissue. The presence of necrotic tissue, hematoma, or foreign bodies within the wound can also become a breeding ground and physical barrier for bacteria, hindering the growth of granulation tissue. The blood supply to the wound is crucial. If the suture tension is too high, or if the wound is located in a poorly vascularized area (such as the distal lower extremities), local ischemia and hypoxia will directly lead to a decrease in cellular repair capacity. Furthermore, the type of wound also matters; severe crush injuries and heavily contaminated wounds inherently heal less effectively than clean cuts.
Does the patient's health condition affect healing ?
Without key nutrients like protein, vitamin C, and zinc, the body cannot synthesize enough collagen to build the repair scaffold. Chronic diseases have a far-reaching impact. In diabetic patients, the high blood sugar environment impairs white blood cell function and microvessels, significantly delaying healing; anemia or hypoproteinemia leads to insufficient oxygen and nutrient delivery; patients with autoimmune diseases or those using immunosuppressants or glucocorticoids long-term experience suppressed immune and inflammatory responses, resulting in decreased repair capabilities. Age is also a factor; older adults generally have weakened cell regeneration and blood circulation, leading to slower healing. Unhealthy lifestyle habits, such as smoking, cause nicotine to strongly constrict blood vessels, severely reducing blood supply to the wound area.
What problems can arise from improper postoperative care?
Even if the surgery is successful, improper aftercare can ruin everything. Excessive moisture or maceration of the wound, such as prolonged soaking in sweat or exudate, softens the skin barrier, making it highly susceptible to infection. Conversely, excessive dryness and crusting can hinder the migration of epidermal cells from the edges to the center. Inappropriate application of ointments or use of home remedies can irritate the wound or cause allergic reactions. Premature or excessive local activity, especially traction on the wound area, increases suture tension, potentially leading to wound dehiscence or internal bleeding.
How can I tell if there's a problem with wound healing?
In the initial postoperative period, there may be mild redness, swelling, heat, and pain, which gradually subsides. The wound edges are well-aligned, and there may be a small amount of clear or slightly bloody exudate. If the following occurs, it may indicate a problem: The redness, swelling, heat, and pain continue to worsen, or reappear after initial relief; increased wound exudate, turning yellowish-green and purulent, or accompanied by a foul odor; separation or dehiscence of the sutured wound edges, or exposure of internal tissue; blisters, severe rashes, or blackening of the skin around the wound; or stagnation of healing, with the wound showing no signs of shrinking or epithelialization beyond the expected time. If any of these signs appear, you should return to the hospital immediately for evaluation by a doctor.
What should you do if a wound is not healing well?
If a wound is not healing well, do not panic or self-medicate; seek professional medical help immediately. The doctor will assess the underlying cause and take targeted measures. If it is infected, thorough debridement, open drainage, and the use of sensitive antibiotics based on bacterial culture results are necessary. If hematoma or necrotic tissue is present, some sutures may need to be removed for cleaning. For wounds with poor blood supply, it may be necessary to improve local circulation or use special dressings that promote angiogenesis. For malnourished patients, a nutritionist will intervene to develop an intensive nutritional support plan. The doctor may also choose modern wound care techniques such as negative pressure wound therapy, growth factors, or new functional dressings to promote healing, depending on the situation. Simultaneously, patients must strictly manage underlying conditions, such as controlling blood sugar, and absolutely abstain from smoking.
For more information on Innomed®Silver Ion Dressing Foam, Refer to the Previous Articles. If you have customized needs, you are welcome to contact us; You Wholeheartedly. At longterm medical, we transform this data by Innovating and Developing Products that Make Life easier for those who need loving care.
Editor: kiki Jia

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








