Chronic wound infection is a major obstacle to wound healing, and understanding the distribution characteristics of its pathogens is of great significance for clinical treatment. Due to the long course of the disease and the unique tissue environment, the bacterial composition of chronic wounds is significantly different from that of acute wounds.

What are the common pathogens of chronic wounds?
Gram-positive cocci are the most common pathogens in chronic wounds. Staphylococcus aureus is most commonly detected, with the proportion of methicillin-resistant Staphylococcus aureus increasing annually. Staphylococcus epidermidis, as an opportunistic pathogen, can cause serious infections in immunocompromised patients. Enterococcus faecalis and Enterococcus urocytogenes are commonly found in patients with diabetic foot ulcers and pressure sores.
Gram-negative bacilli also play a significant role in chronic wounds. Pseudomonas aeruginosa prefers moist environments and is prevalent in diabetic foot and venous ulcers. Escherichia coli and Klebsiella pneumoniae are often derived from the patient's own intestinal flora. Proteus and Enterobacter species are commonly found in patients with poor hygiene.
Anaerobic bacteria thrive in deep tissues and necrotic tissue. Bacteroides fragilis is a common Gram-negative anaerobe. Clostridium perfringens can cause severe tissue necrosis. Peptostreptococcus is a representative Gram-positive anaerobe.
What are the characteristics of the bacterial flora distribution in different wound types?
Diabetic foot ulcers are primarily mixed infections, with Staphylococcus aureus and Pseudomonas aeruginosa often coexisting. Anaerobic bacteria are more frequently detected in deep tissue infections. Multidrug-resistant bacteria are a particular concern in diabetic foot patients.
Venous ulcers are commonly found with Staphylococcus epidermidis and Streptococcus. Gram-negative bacilli are relatively rare, and the bacterial diversity is less diverse than in diabetic foot ulcers.
Pressure ulcers are associated with diverse bacterial species, which are correlated with the patient's length of hospital stay and history of antibiotic use. Enterococcus faecalis and Enterococcus urinaria are frequently detected. Anaerobic bacteria are common in deep pressure ulcers.
Burn wound infections are mainly caused by Pseudomonas aeruginosa and Staphylococcus aureus. Fungal infections are more common in patients who have been taking broad-spectrum antibiotics for a long time.
What are the factors that affect the distribution of pathogens?
The duration of a wound affects the composition of the bacterial flora; the longer the course, the more complex the bacterial species. A history of antibiotic use can alter bacterial selectivity and promote the growth of drug-resistant bacteria. Patients with underlying diseases, such as diabetes, can influence the local microenvironment. Blood supply to the wound site influences the ratio of aerobic to anaerobic bacteria. Exposure to the hospital environment increases the risk of nosocomial infection with drug-resistant bacteria. Patients' personal hygiene habits influence the bacterial flora.
How to accurately identify pathogens?
Wound secretion culture is a basic testing method, but the timing and method of sampling must be carefully considered. Tissue biopsy culture results are more reliable and can reflect the extent of deep tissue infection. Molecular biological methods such as PCR can rapidly detect specific pathogens. Gene sequencing technology can comprehensively analyze the bacterial flora. Antimicrobial susceptibility testing is crucial for guiding antibiotic selection.
Methods for chronic wound infection?
Select targeted antibiotics based on drug sensitivity results, avoiding empirical medication. Consider the drug's ability to penetrate wound tissue to ensure effective concentration. Consider the combined use of antibiotics to enhance antimicrobial efficacy. Adequate treatment courses should be used, but unnecessary long-term medication should be avoided. Topical antimicrobial agents, such as silver-containing dressings, can be used as an adjunct. Regularly evaluate efficacy and adjust the regimen promptly.
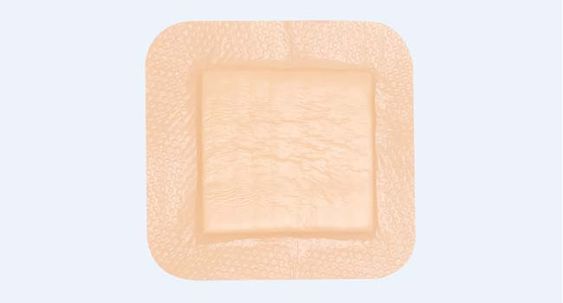
For more information on Innomed@Silicone Foam Dressing Non-Bordered.Refer to the Previous Articles. If you have customized needs, you are welcome to contact us; You Wholeheartedly. At longterm medical, we transform this data by Innovating and Developing Products that Make Life easier for those who need loving care.
Editor: kiki Jia

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








