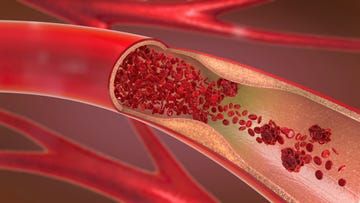
Peripheral arterial disease (PAD) is a pathological condition characterized by restricted blood flow in the extremities, most commonly in the lower extremities. This condition can significantly impair wound healing and complicate treatment. Understanding the impact of PAD on wound healing and implementing targeted care measures are crucial for improving patient outcomes.
What is peripheral arterial disease?
Peripheral arterial disease (PAD) is a disease process in which atherosclerosis leads to narrowing or occlusion of arteries in the extremities. The lower extremities are more commonly affected than the upper extremities, with typical symptoms including calf pain during walking, coolness of the affected limb, and pale skin. As the disease progresses, rest pain, tissue loss, and non-healing wounds may develop. Diabetics, smokers, those with hypertension, and the elderly are at high risk. Diagnosis is based on tests such as ankle-brachial index measurement, vascular ultrasound, and arteriography.
How does peripheral arterial disease affect wound healing?
Reduced arterial blood flow directly leads to inadequate tissue perfusion, limiting oxygen and nutrient supply. Metabolic waste accumulates faster than it can be cleared, impacting normal cellular function. Leukocyte chemotaxis and phagocytosis are impaired, reducing resistance to infection. Fibroblast proliferation and collagen synthesis are slowed, hindering granulation tissue formation. Epithelial cell migration is slowed, prolonging wound closure. Neuropathy reduces the patient's wound perception, potentially delaying treatment.
How to identify wounds associated with peripheral arterial disease?
These wounds are typically located in distal areas with poor blood supply, such as the toes and heels. The wound margins are neat, the base is pale or yellow, and granulation tissue is sparse. Exudate is usually minimal, and the skin surrounding the wound is smooth and shiny, with hair loss. Signs of poor circulation, such as decreased skin temperature and skin color change, are also present. Patients often describe pain at rest, which is aggravated by raising the affected limb and relieved by lowering it. Palpable arterial pulses may be weakened or absent.
Key points in wound assessment for patients with peripheral arterial disease?
A comprehensive assessment should include examination of vascular status and measurement of the ankle-brachial index and toe-brachial index. Wound characteristics should be assessed, noting size, depth, tissue type, and exudate. The surrounding skin should be inspected, noting color, temperature, edema, and hair distribution. The patient's pain level and nature should be assessed, and the impact on quality of life should be assessed. The patient's general condition should be assessed, including nutritional status and comorbidities. The patient's social support system and self-care abilities should be assessed.
What are the special requirements for wound care in patients with peripheral arterial disease?
The primary priority is to improve local blood flow and avoid using vasoconstrictive medications. Keep the wound moderately moist, but avoid excessive moisture that could macerate the surrounding skin. Choose a dressing that does not damage new tissue, avoiding products with excessive adhesion. Protect the surrounding skin to prevent new wounds. Control infection, but avoid using cytotoxic disinfectants. Maintain a suitable temperature, avoiding local overheating or overcooling.
How to improve local blood circulation?
Quitting smoking is the most important measure to improve circulation, as nicotine directly causes vasoconstriction. Moderate activity helps establish collateral circulation, but excessive exertion should be avoided. Avoid wearing tight shoes and socks to prevent further constriction of blood flow. Keep the affected limb in a hanging position to allow gravity to promote blood flow. Avoid local cold, as cold can exacerbate vasoconstriction. Use vasodilators under a doctor's guidance.
Which dressings are suitable for peripheral arterial disease wounds?
Hydrogel dressings provide a moist environment and promote autolytic debridement. Alginate dressings are suitable for wounds with low to moderate exudate. Foam dressings provide good thermal insulation and absorbency. Antimicrobial dressings, such as silver-containing dressings, can control bacterial loads. Avoid dry dressings that remove excess moisture. The frequency of dressing changes should be determined by the amount of exudate and should be performed frequently.
For more information on Innomed®Hydrogel Dressing Tubular, refer to the Previous Articles. If you have customized needs, you are welcome to contact us; You Wholeheartedly. At longterm medical, we transform this data by Innovating and Developing Products that Make Life easier for those who need loving care.
Editor: kiki Jia

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








