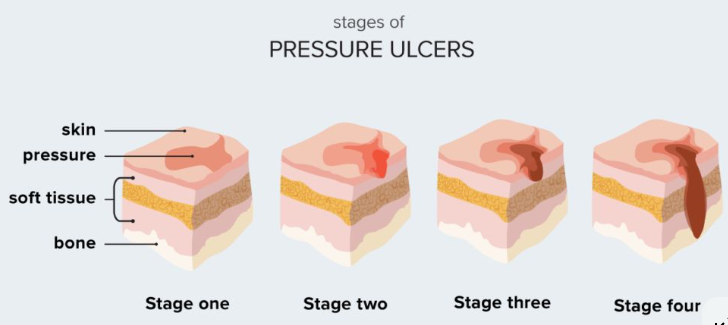
Pressure ulcers are skin and subcutaneous tissue injuries caused by prolonged pressure on localized areas, and are common in people with limited mobility. Proper dressing changes are crucial for promoting pressure ulcer healing; this involves not only technical skill but also a systematic nursing process.
Dressing selection :
For stage I pressure ulcers, transparent film dressings are suitable for easy observation. For stage II pressure ulcers with minimal exudate, hydrocolloid dressings provide a moist environment. For stage III and IV pressure ulcers with significant exudate, foam dressings or alginate dressings are more appropriate. For infected wounds, consider using silver-containing dressings. The dressing should extend 2-3 cm beyond the wound edge. When applying, smooth the dressing from one side to the other, avoiding wrinkles. Use adhesive tape or bandages if necessary.
Preparations before changing dressings :
Observe the stages of pressure ulcers: Stage I is characterized by intact, red skin; Stage II presents with blisters or superficial ulcers; Stage III involves full-thickness skin loss; and Stage IV involves deep lesions affecting the muscles and bones. Measure the size and depth of the wound and record any undermining or sinus tracts. Assess the color, amount, and odor of exudate. Assess the patient's pain level and administer analgesics pre-emptively if necessary. Check the patient's overall nutritional status, as this is fundamental to healing. Prepare sterile dressing packs, appropriate dressings, saline solution, and disinfectants.
Dressing change procedure :
Assist the patient to a comfortable position that fully exposes the wound. Place a waterproof pad under the wound to prevent soiling the sheets. The operator washes hands and puts on sterile gloves. Adjust the lighting to ensure clear observation of wound details. Explain the procedure to the patient and obtain their cooperation.
Cover the wound with sterile gauze and clean the surrounding skin first. Disinfect in a circular motion from the inside out, extending 5 cm beyond the edge of the dressing. Remove the gauze and observe the inside of the wound. Use a sterile syringe to draw up saline solution and flush the wound under appropriate pressure. Flushing from one end of the wound to the other ensures that all necrotic tissue and foreign bodies are removed. For stubborn necrotic tissue, debridement glue or mechanical debridement may be necessary. After flushing, blot the skin around the wound dry with sterile gauze and keep it dry.
After changing the dressing:
Immediately after dressing change, implement decompression measures. Use an air mattress or pressure-reducing mat, assisting the patient to turn over every two hours. Adopt a 30-degree lateral decubitus position to avoid direct pressure on bony prominences. When in a wheelchair, lift the hips every 15 minutes to reduce pressure. Keep bed sheets smooth and dry, avoiding wrinkles that cause friction. Regularly check skin condition, especially bony prominences. Observe the wound for any leakage and change wet dressings promptly. Observe the skin around the wound for maceration or allergic reactions. Assess changes in pain and record the effectiveness of analgesics. Monitor body temperature changes for early detection of signs of infection. Record changes in wound size and depth to assess healing progress. Observe the patient's overall condition, including mental state and appetite.
Pressure ulcer dressing changes are a comprehensive nursing process requiring skill, patience, and a systematic approach. Most pressure ulcers can be improved through standardized dressing changes, effective pressure relief measures, and comprehensive nutritional support. The key lies in early prevention, timely intervention, and continuous management. The collaborative efforts of healthcare professionals, patients, and their families are fundamental to successful treatment. Assist the patient to a comfortable position that fully exposes the wound. Place a waterproof pad under the wound to prevent soiling the sheets. The operator washes hands and wears sterile gloves. Adjust the lighting to ensure clear observation of wound details. Explain the procedure to the patient and obtain their cooperation. For more information on Innomed® Silicone Foam Dressing Sacrum , please refer to the previous articles. If you have customized needs, you are welcome to contact us; you wholeheartedly. At long-term medical, we transform this data by innovating and developing products that make life easier for those who need loving care.
Editor: kiki Jia

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








