Why do foot wounds never heal?
When a foot wound fails to heal for weeks or even months, repeatedly becoming infected and spreading, it's often more than just a skin problem. In many cases, these slow-healing foot wounds are a serious complication of peripheral artery disease (PAD). PAD refers to atherosclerosis in the arteries of the limbs, especially the lower limbs, leading to narrowing or blockage of blood vessels and severely reduced blood flow. Without sufficient oxygen and nutrients, the foot tissues are like soil deprived of water, almost losing their ability to repair themselves. Even a minor abrasion, blister, or small injury from trimming nails can rapidly worsen in an ischemic environment, developing into a chronic ulcer or even gangrene.
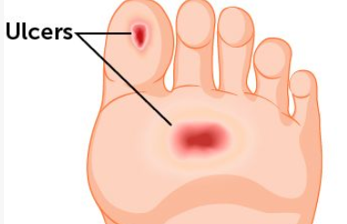
How to identify foot wounds associated with peripheral artery disease?
Foot wounds caused by peripheral artery disease have some typical characteristics. These wounds are usually located at the tips of the toes, heels, or bony prominences, as these areas are the extremities of blood supply. The wounds appear pale or dark red, with a dry base, little or no granulation tissue growth, and are often covered with yellow or black necrotic tissue. Patients usually feel coldness and sensitivity in the affected foot, the skin becomes smooth, thin, and shiny, and hair loss occurs. A key feature is pain, especially rest pain, that is, a deep aching, tingling, or burning sensation in the foot even when not walking or at rest, which often worsens at night and requires leg drop for relief. The dorsalis pedis artery pulse is often weak or absent upon palpation.
Why does peripheral artery disease cause wounds to heal slowly?
Wound healing is a process highly dependent on blood flow. When arteries narrow or become blocked, it triggers a series of chain reactions. First, the quality of oxygen and nutrients delivered to the wound area is severely insufficient, preventing cells from effectively proliferating and migrating to repair the damage. Second, immune cells and antibiotics fighting infection cannot effectively reach the lesion through the bloodstream, and even minor infections can quickly develop into severe ones. Third, metabolic waste and toxins cannot be cleared in time, accumulating locally and further inhibiting healing. Finally, ischemia itself can lead to nerve damage, making patients less sensitive to pain, pressure, and trauma, easily causing undetected injuries, or making them unable to perceive friction from ill-fitting shoes and socks, thus subjecting the wound to constant external force and hindering healing.
How to effectively assess blood supply to the lower limbs?
When peripheral artery disease is suspected, a professional vascular assessment is crucial. Doctors typically perform a thorough physical examination, including palpating and comparing the strength of arterial pulses in both feet, auscultating for vascular murmurs, and checking skin temperature, color, and hair growth. Ankle-brachial index (ABI) measurement is the most basic non-invasive test, reliably and simply determining the degree of blockage in the lower limb arteries by comparing the blood pressure ratio at the ankle and upper arm. If the ABI is abnormal, further color Doppler ultrasound may be performed to visually examine blood flow velocity and plaque levels within the vessels. For patients requiring surgical intervention, CT angiography or MRI may be necessary to obtain a more precise vascular map. These assessments form the basis for developing the appropriate treatment plan.
What are some comprehensive treatment options for these types of slow-healing wounds?
Treatment must be two-pronged, addressing both the local wound and improving overall blood supply. Revascularization is fundamental; depending on the location and length of the blockage, interventional procedures such as balloon angioplasty and stent placement, or surgical bypass surgery, may be employed, all aiming to restore blood flow to the foot. Local wound care requires professional debridement. With improved blood supply, necrotic tissue should be carefully removed to avoid further damage. Appropriate dressings should be selected based on the wound's characteristics. For ischemic, dry wounds, dressings that maintain moisture and promote autolytic debridement, such as Silver Ion Dressing Foam, should be used. Strict infection control is crucial, potentially requiring the use of sensitive antibiotics based on bacterial culture results. Pain management is also essential; improved blood flow itself alleviates ischemic pain, and analgesics can be used appropriately.
How should patients manage themselves on a daily basis?
Patient self-management is key to preventing new wounds and recurrence. Daily foot checks are essential, using a mirror to examine every nook and cranny, including the soles and between the toes, looking for any tiny abrasions, blisters, or discoloration. Keep feet clean and dry; however, use a non-irritating moisturizer when skin is dry to prevent cracking. Choose loose-fitting, breathable shoes and socks with wide toes and smooth linings to avoid any possible friction or pressure. Absolutely avoid using hot water bottles or electric blankets for warmth, as their dulled senses can easily lead to burns. Strict smoking cessation is crucial; smoking severely constricts blood vessels and is the most important reversible risk factor for peripheral artery disease. Simultaneously, actively controlling blood sugar, blood pressure, and blood lipids is necessary; these systemic management practices are vital for slowing disease progression.
When should you seek immediate medical attention?
Seek immediate medical attention for any of the following warning signs: A foot wound rapidly enlarges or deepens, or a new wound appears. A wound discharges pus, has a foul odor, or develops large areas of redness, swelling, and heat around it, indicating spreading infection. Pain suddenly intensifies, or new, severe pain develops. The foot suddenly turns pale, purplish-black, or dark red. Systemic symptoms such as fever, chills, and palpitations may also occur. These signs may indicate a worsening infection, a new vascular event, or a critical stage of limb ischemia; delaying treatment could lead to amputation or even more serious consequences.
For more information on Innomed®Silver Ion Dressing Foam, Refer to the Previous Articles. If you have customized needs, you are welcome to contact us; You Wholeheartedly. At longterm medical, we transform this data by Innovating and Developing Products that Make Life easier for those who need loving care.
Editor: kiki Jia

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








