Principles of use in the treatment of venous leg ulcers
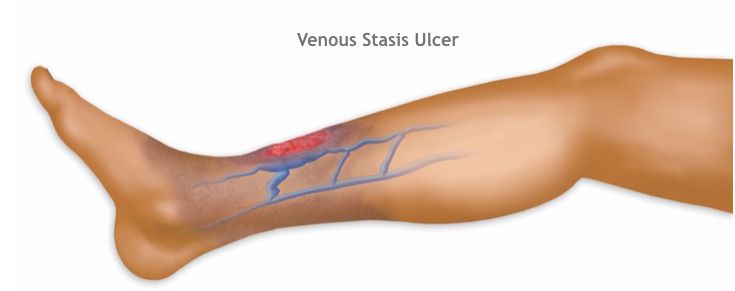
Venous leg ulcers are chronic wounds caused by venous insufficiency in the lower extremities, often prolonging the healing process. How to correctly use antibiotics and disinfectants to control infection and promote healing is a common but often misunderstood issue in the nursing care process. Many patients and their families mistakenly believe that frequent use of strong disinfectants or antibiotic ointments will accelerate healing, but this often has the opposite effect, damaging fragile granulation tissue and even leading to antibiotic resistance.
Why do venous leg ulcers become infected?
Venous leg ulcers, due to local blood stasis, poor tissue nutrition, and low healing capacity, easily become breeding grounds for bacteria. Most chronic wounds have bacterial colonization on their surface, meaning bacteria grow on the wound surface but do not invade deeper tissues or cause a strong immune response; this usually does not require antibiotic treatment. Clinical infection is only considered when bacteria invade living tissue and trigger a persistent inflammatory response, such as increased redness, swelling, heat, and pain, a sudden increase in purulent exudate, a strong odor, or fragile granulation tissue that bleeds easily. Differentiating between colonization and infection is the crucial first step, which usually requires a doctor to make a judgment based on clinical symptoms, sometimes combined with wound secretion culture results.
Why can't systemic antibiotics be used routinely ?
For venous ulcers without signs of systemic infection, routine oral or intravenous antibiotics are ineffective and harmful. Systemic antibiotics cannot effectively penetrate ulcer areas with poor blood circulation, making it difficult to achieve effective concentrations. More importantly, antibiotic abuse can lead to the selection of drug-resistant strains, potentially resulting in a lack of effective treatments when truly serious systemic infections occur in the future. Systemic antibiotics should only be used in patients presenting with systemic infection symptoms such as cellulitis, lymphangitis, and fever, and must be used specifically based on bacterial culture and drug sensitivity results, ensuring adequate dosage and duration of treatment.
Are topical antibiotic ointments effective ?
Similar to systemic medications, topical antibiotic ointments such as mupirocin and fusidic acid have limited use in the treatment of venous ulcers. They are primarily used to treat confirmed local Staphylococcus aureus or Streptococcus infections, and the course of treatment should be short. Long-term, widespread use of over-the-counter antibiotic ointments can also promote local bacterial resistance and may cause contact allergic reactions, leading to dermatitis of the surrounding skin and complicating the problem. Currently, international wound care guidelines generally do not recommend the use of these ointments as routine treatment or prophylactic medication for venous ulcers.
How should disinfectants be used when cleaning wounds ?
Disinfectants such as povidone-iodine, chlorhexidine, and hypochlorite solution are primarily used to clean the intact skin around the wound during dressing changes to reduce the risk of infection. However, the routine use of disinfectants to irrigate open ulcers is controversial. Many disinfectants are cytotoxic to fibroblasts and newly formed epithelial cells, damaging fragile granulation tissue and delaying healing. The correct approach is to irrigate the wound bed with a mild, non-cytotoxic solution, preferably sterile saline or drinking water. If disinfectants must be used to treat heavily contaminated wounds, a less cytotoxic variety should be chosen and diluted to the recommended concentration. After irrigating, the wound should be rinsed again with copious amounts of saline to minimize residue.
How to control bacterial load during nursing care ?
Modern wound management emphasizes controlling bacterial load through physical and chemical methods, rather than simply relying on antibiotics or disinfectants. Autolytic debridement combined with appropriate dressings is the core strategy. Using hydrogel, hydrocolloid, or medical honey dressings can gently remove necrotic tissue, which is a breeding ground for bacteria. For wounds with a high risk of infection or those showing clinical signs of infection, dressings containing sustained-release antibacterial components, such as silver ion dressings, medical honey dressings, or iodine-carrier dressings, can be used. These dressings continuously release antibacterial components locally, effectively reducing bacterial counts, and are less likely to induce resistance. Their cytotoxicity is also far lower than that of liquid disinfectants. Simultaneously, effective pressure therapy is crucial; it improves venous return, reduces edema, and enhances local immunity, fundamentally improving the wound environment and preventing infection recurrence.
The key to controlling infection in the treatment of venous leg ulcers lies in accurately assessing the infection status and implementing interventions that promote a wound-healing environment. Abandoning the outdated notion of overusing antibiotics and disinfectants, and instead adopting a modern wound care model based on standardized pressure therapy, supplemented by advanced functional dressings, and routine saline cleansing, is crucial to creating a genuine chance for these stubborn wounds to heal. When any signs of infection appear, the safest course of action is to consult a professional wound therapist or vascular surgeon to develop an individualized treatment plan. For more information on Innomed® Silver Ion Dressing Foam, refer to the Previous Articles. If you have customized needs, you are welcome to contact us; you wholeheartedly. At long-term medical, we transform this data by innovating and developing products that make life easier for those who need loving care.
Editor: kiki Jia

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








