What is deep tissue pressure injury?
Deep tissue pressure injuries, formerly known as suspected deep tissue injuries, are a special and dangerous type of pressure injury (commonly known as bedsores). The damage begins deep under the skin, caused by intense pressure and shear forces on the soft tissue between the bone and the rigid supporting surface. This type of injury does not start from the skin surface; instead, it first damages deep tissues such as muscles, fascia, or fat, only gradually manifesting on the skin surface later. Because of this, it is extremely insidious and deceptive, often revealing severe tissue necrosis beneath seemingly intact skin. Once the skin shows obvious signs of damage, it often indicates extensive damage deep within the tissue.
How to identify and judge this early ?
Early identification is the greatest challenge in managing deep tissue pressure injuries and is also key to successful management. The initial signs are all on the skin, but the root cause lies deep within. A typical early sign is a persistent, well-defined area of discoloration, either purple or maroon. This area of skin may be intact or accompanied by a congested blister. Upon touch, the skin may feel cool or warm, and the tissue texture may be hard, soft, or doughy. Patients often complain of pain, burning, or itching in the area. These subcutaneous changes signal deep tissue ischemia, hemorrhage, and necrosis. It needs to be carefully distinguished from ordinary bruises, which typically change color and spread over time, while the discoloration of deep tissue injuries does not quickly reverse after pressure is relieved and may rapidly develop into an open wound.
be done correctly after it is discovered ?
The primary and ongoing measure is to completely relieve all pressure on the area using a professional, high-specification pressure-relief mattress and cushion, and to establish a strict, timed turning schedule to ensure the injured area is completely suspended. For intact skin, simply keep it clean and dry, avoiding the use of ointments or massage creams that may cause local dampness. For surface blisters, if the blister skin is intact, it should be preserved as much as possible as a biological dressing to protect the underlying tissue; if the blisters rupture, they must be treated aseptically, cleaned with saline solution, and covered with a high-grade dressing such as a non-adhesive silicone foam dressing to absorb exudate, while closely observing the patient. The most crucial aspect of the entire treatment process is dynamic assessment, with observation at least twice daily, recording changes in skin color, temperature, texture, blister size, and patient sensation, and taking photos for comparison.
How to care for open wounds?
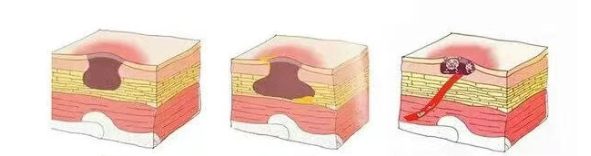
Deep tissue pressure injuries have two possible outcomes. Ideally, with timely and thorough pressure relief, some damage may be reversed, the discolored area gradually absorbs, and the tissue returns to normal. However, more commonly, the damage is irreversible; the deep necrotic tissue eventually liquefies and penetrates the surface tissue, forming a deep, burrowing, or sinus-like open wound. In this case, the wound may be small, but the extent of internal necrosis is far greater than what is visible on the surface, often referred to as a "small wound with a large cauldron." The focus of care shifts to standardized wound management: conservative sharps debridement or autolytic debridement should be performed under the supervision of a medical professional, gradually and in stages, removing necrotic tissue (usually black eschar or yellow necrotic tissue). Depending on the amount of wound exudate, appropriate filling dressings (such as alginate, hydrocolloid fibers, or foam dressings) should be selected for drainage and absorption. If signs of infection are present, antibacterial dressings containing silver or iodine should be used. The entire process must be gradual; a single, thorough debridement should be avoided to prevent excessive trauma.
How can we effectively prevent this from the root cause?
Prevention is far better than cure, especially for such insidious injuries. Prevention strategies should be a multi-layered, systematic approach. Continuous pressure relief is the cornerstone. For high-risk patients (such as those with spinal cord injuries, prolonged bed rest, severe weight loss, or edema), specialized support equipment such as dynamic or static air mattresses must be used, and a strict repositioning procedure every two hours is essential. Reduce shear and friction forces by using sheet-like aids to lift the body when moving the patient, avoiding dragging; keep the head of the bed elevated no more than 30 degrees (unless the patient's condition precludes it). A comprehensive skin assessment should be included in routine care, examining bony prominences and pressure points at least daily under good lighting, especially common sites such as the hip, tailbone, heels, and ischial tuberosities, paying attention to even the smallest color changes. For more information on Innomed® Silicone Foam Dressing, refer to the Previous Articles. If you have customized needs, you are welcome to contact us; You Wholeheartedly. At long-term medical, we transform this data by Innovating and Developing Products that Make Life easier for those who need loving care.
Editor: kiki Jia

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








