What is an acute wound infection?
Acute wound infection refers to a series of local and systemic inflammatory responses triggered in the early stages of wound healing (usually within two weeks of injury) due to the invasion and proliferation of pathogenic microorganisms such as bacteria, exceeding the body's local immune defense capabilities. It is the most common complication of wounds, directly interrupting the normal healing process, leading to delayed wound healing, wound dehiscence, and scar hyperplasia. In severe cases, the infection can spread into the bloodstream, causing sepsis and endangering life.
How can we accurately identify the signs of acute wound infection?
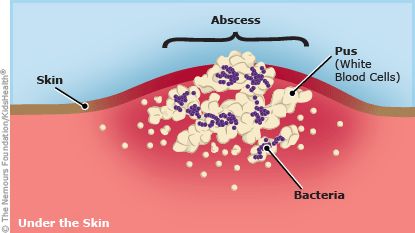
Identifying infection requires combining local signs, systemic symptoms, and the patient's subjective experience. Local symptoms are the most obvious, with the classic four signs being redness, swelling, heat, and pain. Specifically, the redness and swelling around the wound will extend beyond the original wound edge and spread to the surrounding normal skin; the local skin temperature will be significantly higher than the surrounding skin; the pain will not lessen after 48 hours but will continue to intensify, or throbbing pain may occur. Changes in the characteristics of wound exudate are important clues. Normal exudate is clear or slightly bloody, while in infection, the exudate will increase, becoming cloudy yellow or yellowish-green purulent, sometimes accompanied by a fishy or foul odor. The wound base may be covered with yellow necrotic tissue or new necrotic tissue may appear.
What emergency measures should be taken after signs of infection are detected?
If wound infection is suspected, the first step is to ensure adequate drainage. If the wound is superficial and has pus buildup, after cleaning with saline solution, gently absorb the surface pus with sterile gauze. Do not squeeze forcefully, as this may push bacteria deeper. Then, thorough cleaning is necessary. Rinse the wound with plenty of sterile saline solution or a doctor-recommended wound cleaning solution to wash away some bacteria and necrotic tissue debris. After cleaning, leave the wound open and do not cover it with a traditional occlusive dressing temporarily. Apply a doctor-prescribed topical antibiotic ointment (such as mupirocin ointment or fusidic acid cream) and use a soft silicone contact layer dressing . This will keep drainage unobstructed and prevent pus buildup. At the same time, allow the wound to rest and reduce activity, especially avoiding pulling on the wound area.
What professional treatment measures do doctors usually take?
For localized infections, the core procedure is professional debridement. Under sterile conditions, the doctor will use surgical instruments to remove all necrotic tissue and pus from the wound; this is the most effective step in controlling the infection. Simultaneously, wound secretions will be collected for bacterial culture and drug sensitivity testing to accurately identify the causative bacteria and select the most sensitive antibiotic. Depending on the situation, systemic antibiotics, either oral or intravenous, may be prescribed. For local care, advanced functional antibacterial dressings, such as silver-containing dressings, iodine-containing dressings, or medical honey dressings, may be used. These dressings continuously release antibacterial components, effectively controlling the local bacterial load. For wounds that have formed abscesses, surgical incision and drainage may be necessary to establish a patent drainage channel. For certain severe or special infections (such as animal bites or heavily contaminated wounds), tetanus antitoxin or immunoglobulin may also be recommended.
How to effectively prevent acute wound infections?
Prevention is always better than cure. Infection prevention needs to be maintained throughout the entire process from injury to healing. Thorough debridement in the early stages of injury is the cornerstone of prevention; it must be done by rinsing with plenty of saline solution to remove all foreign objects and contaminants. Keep the wound clean and dry daily, and change dressings regularly. If the dressing becomes wet or contaminated with exudate, it should be changed immediately. Choose appropriate dressings. For clean wounds, breathable and waterproof film dressings can be used; for wounds with exudate, choose highly absorbent foam or alginate dressings to maintain a moist healing environment.
For more information on Innomed®Silver Ion Dressing Foam, Refer to the Previous Articles. If you have customized needs, you are welcome to contact us; You Wholeheartedly. At longterm medical, we transform this data by Innovating and Developing Products that Make Life easier for those who need loving care.
Editor: kiki Jia

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体








