Smart wireless wound patch monitors healing progress and infection risk in real time
A research team at RMIT University in Melbourne, Australia, has successfully developed a flexible, Bluetooth-enabled smart wound monitoring patch that provides real-time, multi-parameter monitoring of wound healing and infection risk without removing the dressing. This technology has the potential to significantly improve the treatment experience and reduce the healthcare burden for patients with chronic wounds. The research findings have been published in Advanced NanoBiomed Research.
Chronic wounds, with their difficulty healing and high risk of infection, have long plagued healthcare systems worldwide. According to statistics, approximately 500,000 people in Australia alone suffer from chronic wounds, resulting in approximately $3 billion in annual healthcare expenditures. Traditional approaches rely on frequent dressing changes and clinical examinations, which not only increase patient suffering but also hinder continuous, dynamic monitoring.
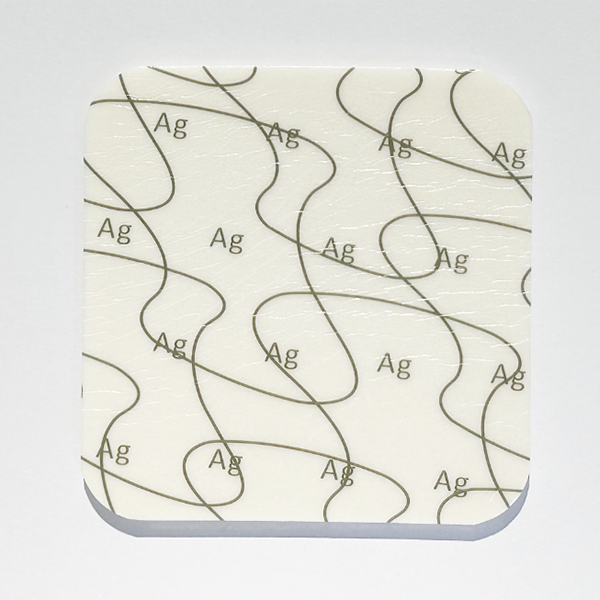
This innovative wearable device, developed by the RMIT team, integrates a high-resistance silicon conductivity biosensor, a potentiometric pH sensor, and a temperature sensor. It can simultaneously detect key inflammatory biomarkers (IL-6 and CRP), pH, and temperature changes. Using Bluetooth technology, the device transmits real-time data to the mobile app "FMM Connect," enabling doctors and patients to remotely monitor wound status, identify problems promptly, and adjust treatment strategies.

The device employs a "triangulation" strategy, enhancing monitoring accuracy through multi-parameter cross-validation. For example, an IL-6 concentration exceeding 45.36 nM or a CRP concentration exceeding 41.67 nM may indicate chronic infection; a pH above 7.4 or a temperature exceeding 38°C may also signal infection or tissue necrosis. Together, these parameters provide a comprehensive and objective assessment of wound healing progress.
Researchers successfully validated the device's performance in the laboratory, including its ability to detect biomarkers in a simulated wound environment, as well as its conformability and flexibility to curved human surfaces. Its modular design allows for the reuse of the electronics and the replacement of the sensor unit with every dressing change, demonstrating its practicality and affordability.
"This device not only reduces unnecessary dressing changes and physical contact, lowering the risk of infection, but more importantly, provides doctors and patients with continuous and objective data support, enabling more precise wound management," said the head of the research team.
This technology, based on RMIT's established high-resistance silicon sensor platform, offers excellent scalability. By adding other biomarker detection modules, it can be expanded to more immediate diagnosis scenarios, such as postoperative recovery monitoring and diabetic foot care.
The industry believes that this innovation provides a more reliable and low-cost solution for smart wound care products, which is particularly suitable for applications in resource-limited or telemedicine scenarios and has significant prospects for clinical transformation.

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体









.jpg.png)

.jpg.png)
.jpg.png)
.jpg.png)


