Children are prone to fever in summer, which can generally be considered from the following aspects:
1. It may be caused by an upper respiratory tract infection. In summer, the baby wears thin clothes. After blowing the air conditioner and fan, it may cause a cold, and it is easy to cause fever after a cold. Second, it may be caused by gastroenteritis. In summer, the general diet is relatively cold, the food is easy to spoil, and the baby's spleen and stomach are weak, which can easily cause gastroenteritis, but gastroenteritis will be accompanied by diarrhea. Third, it may be caused by skin diseases. Such as measles, chickenpox, or baby rash.
Six common problems with children's fever and the correct way of nursing
In clinical work, fever is usually defined as axillary temperature ≥37.3 °C or rectal temperature ≥38 °C. Abnormal body temperature should be regarded as a manifestation of disease. (Forehead thermometer is recommended for children over three years old, and oral temperature measurement is recommended for children over four years old)
Clinically, fever is divided into four categories according to the temperature. Based on the axillary temperature, 37.5-38.0℃ is low fever, 38.1-39℃ is moderate fever, 39.1-40℃ is high fever, and ≥41.0℃ is ultra-high fever.
When children over two months of age have a body temperature of ≥38.2°C with obvious discomfort, drugs can be used to reduce fever.
Acetaminophen is recommended for children over two months of age who need medication to reduce fever, and acetaminophen or ibuprofen is recommended for children over six months of age.
Any antipyretic and analgesic drugs are contraindicated in children under two months of age with fever; the combination or alternate use of acetaminophen and ibuprofen is not recommended
cannot.
During the period of rising body temperature, if the child has symptoms such as chills and shivering, it is appropriate to add clothes to keep the child warm to improve comfort of the child.
During the duration of the fever, because the child's body temperature regulation ability is not perfect, too many or too thick clothes or quilts are not easy to dissipate heat, but may lead to high fever due to heat accumulation in the child's body.
In infants, excessive warmth or stuffing can also lead to dehydration. For children with fever, antipyretic measures should be adopted to improve their comfort of children, and a large amount of clothing should not be added blindly. What should I do?
None of the following physical cooling measures are recommended for antipyretic therapy in young children or children:
Large areas of high-concentration ethanol rubbing, ice water enema, etc., these methods will significantly increase the discomfort of children (chills, goosebumps, crying). ×
Excessive or extensive use of physical methods to cool down the skin by cooling the skin will instead cause the body to counteract the effects of physical cooling by increasing heat production (chills) and further reducing heat dissipation (constriction of skin capillaries, skin goosebumps caused by contraction of pili muscles).
The following physical cooling measures are recommended:
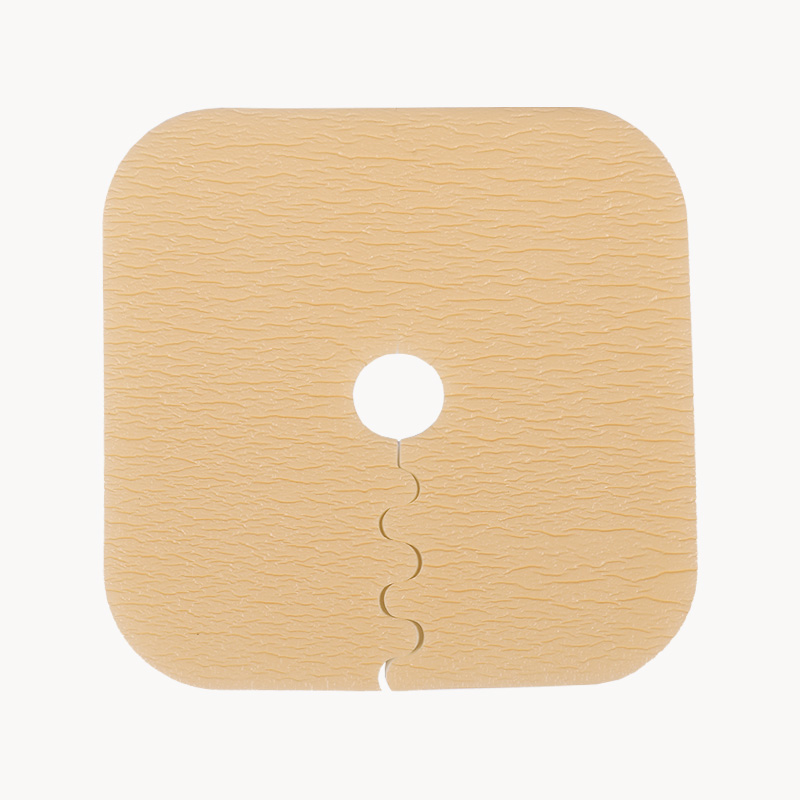
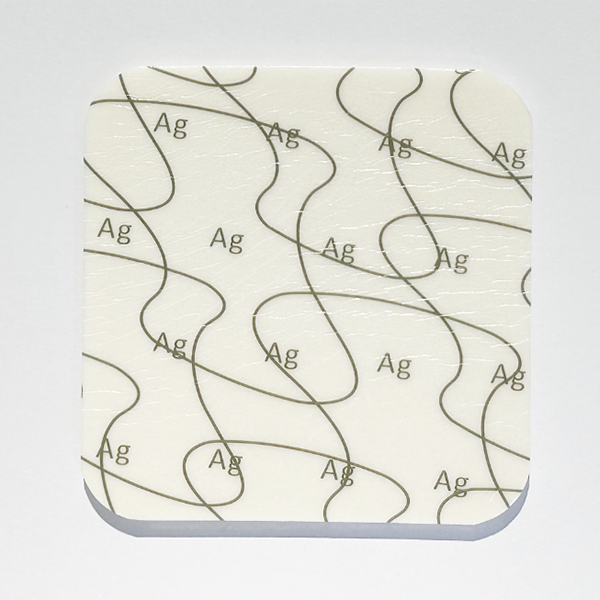
The correct way for children to have a fever includes warm water external application, a warm water bath, and antipyretic patches. √
Apply four or more antipyretic patches to the child's forehead, temples, cervical spine, armpit, popliteal fossa, groin, and other major arteries passing parts, or apply warm water to the child's forehead, take a warm bath for an appropriate time, or reduce the amount of clothing worn. Play the role of physical cooling. Fans and lowering the indoor temperature can also take away heat from the body through conduction, convection, and evaporation so that children with a fever feel comfortable.
When a child has a fever, if it is only manifested as a simple increase in body temperature, normal skin and lips color, moist mucous membranes, lucidity, strong crying, good mental response after fever, no obvious infection lesions, no other accompanying symptoms, no shortness of breath, You can temporarily not go to the hospital, observe and treat at home, and at the same time, you can take physical methods such as drinking more water, taking warm water baths, reducing clothing, and lowering the ambient temperature to reduce fever, monitor changes in body temperature, and administer antipyretic and analgesic drugs if necessary (should be administered between 2 doses). If you have other symptoms, seek medical attention as soon as possible.
If any of the following conditions occur, you should go to the hospital for diagnosis and treatment immediately.
Children younger than three months have been to the foci before fever or suspected exposure to the affected area, unable to eat and drink, have a rash that does not fade, pale or gray or cyanotic, patterned skin, confusion or very unresponsive Poor physical activity, persistent pain or crying, shortness of breath, tachycardia, persistent high fever (>39°C), convulsions, diagnosed with immunodeficiency disease or blood disease, etc.
Uncertain.
In most cases, children with a fever do not need infusion therapy. Whether or not infusion therapy is performed depends on the condition and diagnosis and is not directly related to the temperature.
Indications for infusion therapy in children with acute fever include:
(1) There is a high risk of serious bacterial infection or bacteremia, requiring intravenous antibiotics;
(2) Obvious dehydration and need to be corrected by intravenous fluid rehydration, or there is dehydration manifestation and oral rehydration cannot be performed;
(3) There is an obvious electrolyte imbalance, which needs to be supplemented or corrected intravenous;
(4) There is shock or other critical condition.
In the absence of these conditions, the child is generally in good condition and does not require infusion therapy. Conventional infusion therapy by itself cannot lower body temperature. Summary of home care after fever
(Longterm Medical recommends that you always keep home health care products, and minor injuries and minor patients can do it yourself)
①When a child is found to have a fever; parents should measure the body temperature as soon as possible. It is recommended to use an electronic thermometer for axillary temperature measurement.
②When the child's body temperature is less than or equal to 38.2°C, an alcohol cotton pad can be properly soaked in warm water to wipe the armpits, palms, soles, or back of the feverish child, which is beneficial to promote the gradual decrease of body temperature;
③ After wiping, apply medical antipyretic stickers to the forehead, temple, carotid artery, cervical spine, and other parts of the child. If you want to achieve a rapid cooling effect, you can use professional stickers on the forehead, temple, cervical spine, armpit, popliteal fossa, groin, and other large arteries passing through the site for cooling care.
Other:
Children over two months of age with a body temperature of ≥38.2°C and with obvious discomfort can use antipyretic and analgesic drugs. They should take oral drugs in strict accordance with the dosage recommended in the instructions. After oral administration of antipyretic and analgesic drugs, they will sweat a lot and should be replaced in time. Clothes that make the child comfortable.
After the use of antipyretic analgesics, the body temperature usually begins to drop within 30-60 minutes. If you find that the child continues to be lethargic, has a poor mental response, or has febrile convulsions, you should seek medical help in time.
Poor appetite, sweating, increased breathing, and increased metabolism should make children drink more water, and the diet should be light and easy to digest.
Parents should record the child's body temperature, water intake, diet, frequency of urination and color, etc. This information can help determine the child's status; open windows regularly every day to keep the air fresh, and try to avoid convective wind when ventilating; ensure that the child is adequate rest to promote physical recovery.

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体











.jpg.png)
.jpg.png)


