On June 23, 2025, Stanford School of Medicine announced exciting news that a landmark clinical trial had achieved a major breakthrough. Genetically engineered skin transplants using the patient's own cells successfully healed chronic wounds in patients with severe dystrophic epidermolysis bullosa (EB), revolutionizing the treatment of this rare disease, and are expected to completely change the patient's life trajectory.
Reshaping patients' lives
In this highly anticipated Phase III clinical trial, researchers carefully designed a comparative study plan to strictly compare the wounds of EB patients who received genetic engineering transplants with those who did not receive transplants. The results were impressive. The wound healing effect of the transplanted patients achieved a qualitative leap, and the pain and itching symptoms were also significantly alleviated. This achievement was published in the Lancet, a top international medical journal, on June 23, attracting widespread attention from the global medical community. Previously, the U.S. Food and Drug Administration approved this skin transplantation therapy for EB treatment on April 29, paving the way for its clinical application.
"With our innovative gene therapy technology, we have successfully overcome the most difficult wounds to heal, which often cause unbearable pain to patients," said Jean Tang, MD, PhD, professor of dermatology at Lucile Packard Children's Hospital Stanford University, and lead author of the study. "This is undoubtedly a dream come true for all the scientists, doctors, nurses, and patients involved in this long and arduous research process, and we are proud to be able to make a real difference for patients."
From pain to rebirth
Charlotte Brown, a 20-year-old girl from Birmingham, Alabama, is one of the beneficiaries of this clinical trial. She resolutely decided to participate in the Phase III clinical trial in 2021, and this decision completely changed her life. After receiving the genetic engineering transplant, the severity of her chronic wounds that had tortured her for a long time was significantly improved, and she was even able to continue her beloved job as a pharmacist and regain her confidence and enthusiasm for life.
"This has really changed my life," Brown said. "I feel so much better." She once painfully described the feeling of her EB wounds without skin grafts, "It was like it was burning all the time, almost like it was submerged in lava." The transplant surgery in the clinical trial was like a ray of light, illuminating her path to recovery, helping several large open wounds on her thighs, buttocks, abdomen, and back to gradually heal, and now these wounds are mostly or completely closed. "I'm not in so much pain anymore," Brown said. "I don't have to wear so many bandages, so I feel a lot more relaxed."
Brown's experience is not an isolated case. She is just one of 11 patients who participated in the study. Most of these patients received new treatments in multiple parts of their skin, and their wound healing and quality of life were significantly improved. These successful cases fully demonstrate the potential and value of genetically engineered skin transplantation therapy, bringing hope to more patients.
Innovative Technology:
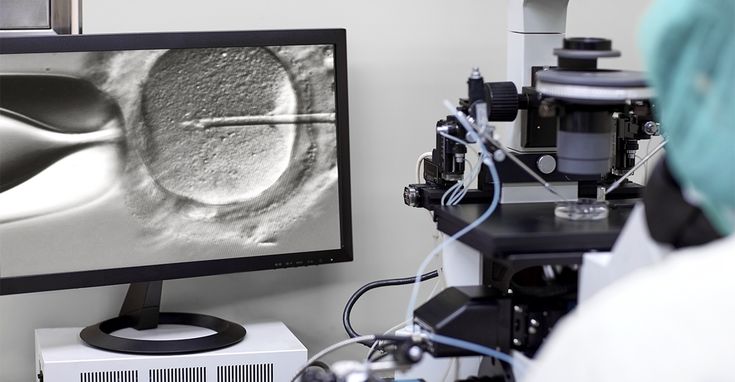
The new skin transplant technology is the result of more than 20 years of dedicated research at Stanford School of Medicine, and it embodies the efforts and wisdom of countless scientific researchers. The researchers collected a small biopsy sample from the patient's uninjured skin, took it to the laboratory, and used advanced retroviral technology to accurately introduce the modified type VII collagen gene COL7A1 into the skin cells. These genetically modified cells were cultivated in the laboratory into skin pieces the size of a credit card. After about 25 days of careful cultivation, plastic surgeons precisely sutured these genetically modified skins to the patient's wounds. Because each transplanted skin is taken from the patient's own skin, it can provide healthy skin that perfectly matches the patient's own immune markers, thereby effectively preventing the rejection of the transplanted skin and ensuring the safety and effectiveness of the treatment.
In this phase III study, 11 patients with recessive dystrophic EB were included, all of whom were at least 6 years old. The study cleverly compared pairs of wounds in similar locations on the same patient: one wound in each pair was treated with a genetically engineered skin graft, and the other wound was treated with conventional care. 24 weeks after the transplant, 81% of the wounds in the treatment group were at least half healed, while the wound healing rate in the control group was only 16%; 65% of the wounds in the treatment group were at least three-quarters healed, while the wound healing rate in the control group was only 7%; and 16% of the wounds in the treatment group were completely healed, while the wounds in the control group were completely healed. In addition, the patient's feedback on pain, itching, and blistering in the transplanted area was significantly better than that in the control group wounds, a series of data that strongly demonstrated that the transplanted area was significantly improved compared with the control group wounds. The study reported that the skin grafting surgery was safe and reliable, and the treatment-related adverse events experienced by patients were not serious, which laid a solid foundation for the widespread use of this therapy.
The research team is not resting on its laurels. They plan to follow up the patients participating in the clinical trial for up to 15 years to fully test the continued effectiveness of the transplanted flaps. The researchers are hopeful that these flaps will be able to effectively reduce the long-term risk of infection and skin cancer at the transplant site and provide long-term health protection for patients. "It's important to let patients know: this may give you a chance to be reborn," Brown said affectionately, "If you're afraid you can't do it, it will help you get closer to a normal life, or make your quality of life better than before." Mr. Tang is looking to the future, and he looks forward to seeing how these therapies will work when applied to very young patients. "I hope that if these patients were diagnosed as infants and started using gene therapy gel, perhaps there wouldn't be a large wound," Tang said, "but if the gel doesn't work and the wound does expand, then skin grafting is the right treatment. I hope that their disease life expectancy curve can be changed, and the pain will be reduced."
The Phase 3 study was funded by Abeona Therapeutics Inc., and scientists from the VA Palo Alto Healthcare System, the University of Massachusetts Chan School of Medicine, Abeona Therapeutics Inc., and the University of Colorado Anschutz Medical Campus worked together to contribute their wisdom and strength to this medical breakthrough.
Source:
Stanford School of Medicine
Journal reference:
Tang, JY, et al. (2025). Prademagene zamikeracel for the treatment of wounds with recessive dystrophic epidermolysis bullosa (VIITAL): a two-center, randomized, open-label, within-patient-controlled phase 3 trial. Lancet. doi.org/10.1016/S0140-6736(25)00778-0 .

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体









.jpg.png)
.jpg.png)
.jpg.png)



