A research team at the Center for Disaster Medicine and Traumatology at Linköping University in Sweden has recently developed a novel "injectable skin" technology. Using 3D printing, they fabricate a gel structure containing living cells, offering new possibilities for treating severe burns and wounds. The research has been published in the journal Advanced Healthcare Materials.
Limitations of traditional burn treatment
Currently, burns are typically treated with a thin layer of epidermal graft. While this method can help wound healing, it can easily lead to scar contracture and compromise skin function. While dermal grafts can improve recovery, their clinical application is limited by the significant surgical trauma and limited donor resources.
"The complex structure of the dermis is difficult to fully replicate in the laboratory," said Johan Junker, associate professor of plastic surgery at Linköping University and a member of the research team. "Our approach is to provide a scaffold that allows the patient's own regenerative abilities to take effect."
Precisely fit the wound.

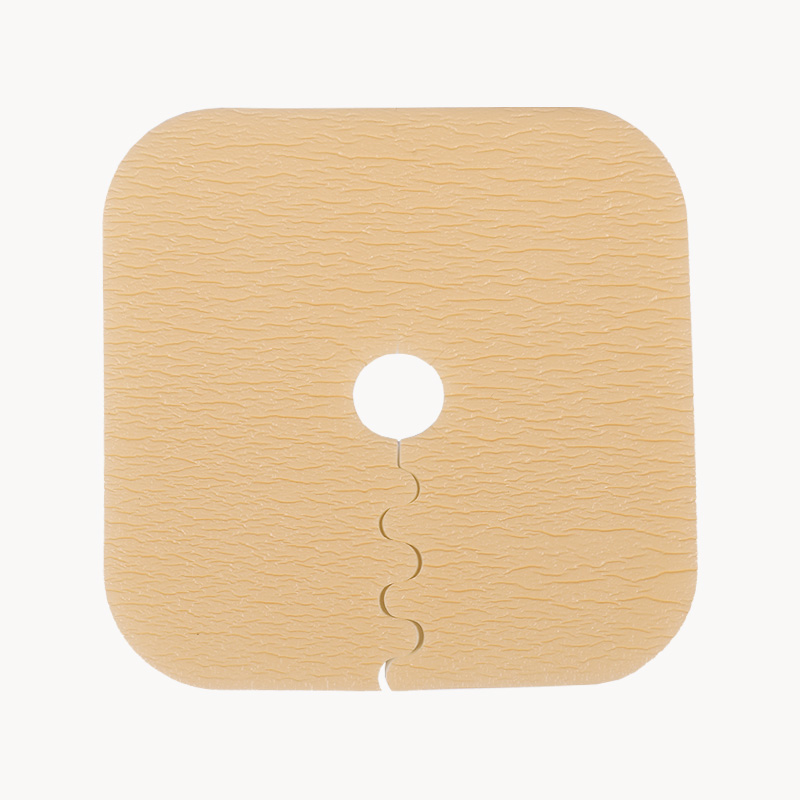
The research team used microporous gelatin beads as a cell carrier. This material, made of a collagen-like substance, is effective in culturing fibroblasts, the primary cell type in the dermis. To ensure the gel's stable adhesion to the wound surface, the researchers mixed the gelatin beads with hyaluronic acid gel and cross-linked them using a "click chemistry" technique, ultimately creating a biomaterial with unique rheological properties.
"This gel becomes liquid under slight pressure and can be precisely injected into the wound using a syringe. When the pressure is removed, it quickly returns to its gel state, forming a stable structure on the wound," explained Daniel Aili, professor of molecular physics.
Animal experiments show good results.
In experiments with mice, the researchers implanted the 3D-printed cell gels subcutaneously and observed the following results:
- High cell survival rate: Transplanted cells continue to secrete dermal matrix components such as collagen and elastin, which help to repair the skin.
- Angiogenesis: A vascular network spontaneously forms inside the gel, solving the problem of insufficient oxygen supply in traditional tissue engineering.
- Potential for personalized treatment: Only a small amount of the patient's own skin cells is needed to expand and culture enough transplants, reducing the risk of rejection.
"This technology has the potential to advance dermal regeneration from laboratory research to clinical application," Juncker said. "We are not only focused on wound closure, but also on achieving functional skin restoration."
The research team also developed a high-water-content elastic hydrogel thread, with a water content of up to 98%. This material exhibits excellent plasticity and knottability, allowing it to be used to construct micro-perfusion channels, offering a new solution to the problem of vascularization in tissue engineering. Lars Kölby, Professor of Plastic Surgery at Sahlgrenska University Hospital in Gothenburg, stated, "This approach could revolutionize the design of complex tissue engineering."
This research was funded by the Elin Persson Foundation, the European Research Council (ERC), and the Knut and Alice Wallenberg Foundation. The research team is currently conducting large animal studies to further validate the safety and efficacy of this technology. They are also exploring the potential application of hydrogel threads in the treatment of chronic wounds, such as diabetic ulcers.
Further development of this technology may lead to more efficient and personalized treatment options for patients with burns, trauma, and chronic wounds.

 English
English عربى
عربى Español
Español русский
русский 中文简体
中文简体













.jpg.png)
.jpg.png)


